Helping Someone in the Face of Suicidal Risk #217 (Part II) ⭕️
Postcards, alcohol, unspoken associations, paradoxical positivity, and our need for each other.
Here’s Part II on the topic of working with people who have suicidal risk.
In case you missed some of the resources based on Stacey Freedenthal’s book, here is the link to Part I.
When was the last time you sent a postcard?
A hospital in New South Wales Australia conducted a randomised controlled trial to see if a piece of 3.5 x 5 inch cardstock paper mailed to patients after being admitted to their hospital for suicidality, can reduce future suicide attempts.
See the original study.
This is what the postcard looks like:Not exactly something you would call fancy or sophisticated, isn’t it?
Here’s what they found:A postcard sent to patients at intervals1 sent at after discharge for an episode of deliberate self poisoning, compared to a control group, the postcard group nearly halved the number of repeat episodes in 12 months.
This low-cost intervention maintained even at a 24-month follow-up (see the follow-up study).
Why did this help? I suspect it sends a signal that someone is thinking of them, that ‘you are on my mind,’ even when they feel isolated.
The research on suicide from Matt Nock’s lab is worth paying attention to. This particular study intrigued me for a long time. (Full text on ResearchGate)
Performance on an implicit association test (IAT)2 prospectively predicted actual suicide attempts during the 6 months following the emergency department visit among participants who had a history of suicide attempts at baseline.
The researchers were able to predict a 6-fold increase in the odds of making a suicide attempt in the next 6 months.
The key finding to me is that it was not the explicit associations with death/suicide, but the implicit thoughts that “may represent one of the final
steps in the pathway to suicide that is activated when a person
is deciding how to respond to extreme distress.”
Nock and colleagues noted from previous studies that a high percentage of people who die by suicide may explicitly deny suicidal thoughts.
There was also a lack of association between clinician’s prediction and subsequent suicidal behaviour.
Alcohol Use and Death by Suicide
This is a meta‐analysis of 33 longitudinal studies, examining if alcohol use is a risk factor for death by suicide.
While the finding is not surprising, the degree to which it is, is striking.
“Alcohol use was associated with a 94% increase in the risk of death by suicide.”
This study is worth noting. Suicide notes were found to use less distress language, more positive emotional language than, blogs about depression and suicidal ideation.
Clinically, we have to pay attention when the emotional language changes with our clients.
We Believe Each Other Into Being
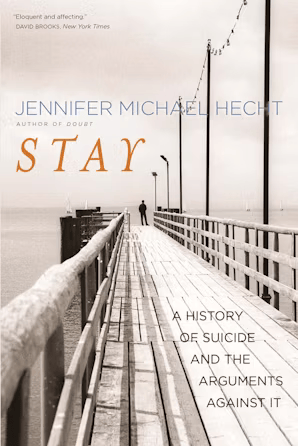
Listen to this interview with Jennifer Hecht.
As a philosopher, historian, and poet Hecht traced how Western civilisation has at times demonized those who commit suicide, at times celebrated it as a moral freedom. She proposes a reframed cultural conversation, based not on morality or rights but on our essential need for each other.
If this gets you interested, read her book, Stay.
P/S: If this was hard to read, even if you are a helping professional, do reach out for support in your local area. Suffering is wasted when we suffer alone.
Daryl Chow Ph.D. is the author of The First Kiss, co-author of Better Results, The Write to Recovery, Creating Impact, and the latest book The Field Guide to Better Results. Plus, the new book, Crossing Between Worlds.
You might be interested in my other Substack, Full Circles: Meditations on the Inner and Outer Life.
A total of eight postcards sent at 1, 2, 3, 4, 6, 8, 10, and 12 months after discharge.
Mahzarin Benaji co-authored a book called Blindspot, if you are interested in learning more about implicit tests.