Three Surprising Facts About Psychotherapy You and Your Doctors Need to Know
Updates from
The Mind of Health
Cutting Edge Updates for Clinicians and Patients, Bridging the Divide Between Mind and Matter
In the 07/08/2016 edition:
*|MC:TOC|*
Three Surprising Facts About Psychotherapy You and Your Doctors Need to Know
By darylchow on Jul 08, 2016 04:50 pm
With the help of a hearing aid, boy hears for the first time.
This post is written for those who are thinking about seeking help. Maybe you are wondering, unsure of who to go to and what to look out for. Or maybe you just need a reason to give yourself a shot at therapy/counselling before you take a psychotropic drug for your emotional problems.
Here’s what you need to know.
Effectiveness of Psychotherapy
Based on more than 50 years of psychotherapy outcomes research, the average treated person better off than 80% of those who did not receive treatment (Miller, Hubble, Chow, & Seidel, 2013; Wampold & Imel, 2015). This is equivalent to an effect size (i.e., magnitude of change) of 0.8, which is considered as a large effect.
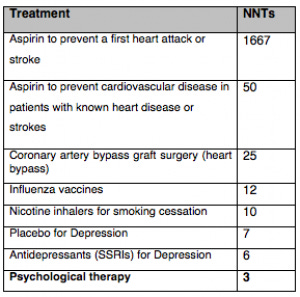
Conventionally used in evidence based medicine, the number need treat refers to the number of patients needed to receive treatment in order to experience a positive outcome relative to untreated patients. To put into context, here are the following NNTs for various treatments (Note: smaller numbers indicate more effective a treatment):
Surprising Fact #1: Psychotherapy is more effective than most medical treatments with lesser side-effects.
Psychotherapy has been shown to reduce the use of medications, consultations with primary-care physicians, length of inpatient stays, and general health care expenditures by 60% to 90% (Chiles, Lambert, & Hatch, 1999; Kraft, Puschner, Lambert, & Kordy, 2006).
More recently, based on a real-world study of over 22,000 clients in a five-year period, the data suggests outpatient psychotherapy has a large reduction of work disability days (41.8%), hospitalisation days (27.4%), and inpatient costs (21.5%). In terms of long-term effects, the researchers found that the year after therapy, the number of work disability days was lower (23.8%) (Altman et al., 2016).
From an investment standpoint, for every dollar spent in terms of care, $2 to $3 are returned! And for every dollar spent in terms of care, it resulted in 3 to 5 times of benefit for health returns (Chisholm et al., 2016). It’s hard to find any other area in healthcare for such returns, with few side-effects.
Are you spinning by now?
Here’s the gist: Psychological treatment is an effective treatment, when delivered in a manner that is cogent with the person, by someone with expertise in a given domain (e.g., depression, anxiety, trauma related, relational issues, psychosomatic complaints).
Why It’s Important for Therapists to Monitor Outcomes
Given the resounding evidence in our field, one of the biggest scandals in psychotherapy is terminating treatment before the experience of benefit. Clinicians typically achieve robust outcomes with clients who are engaged in the process, but too many discontinue from treatment.
Surprising Fact #2: Therapist average about 47% in client dropout rate.
A quick way to resolve this issue is to systematically elicit formal patient feedback. This is done by using brief measures that tracks the progress and engagement level of each patient at each session. More than a dozen RCTs involving more than 10,000 diverse consumers have found that adopting a routine outcome monitoring (ROM) into their clinical practice, reduces dropout rates by half. In addition, the practice of ROM doubles the “effect size” of treatment, compared to not systematically monitoring and feedbacking progress with patients. Furthermore, evidence suggest that the more effective therapists seem to be able to weave in the feedback beyond just as a measurement tool (Chow et al., 2016; Miller, Hubble, Chow, & Seidel, 2016).
My Outcomes: For close to a decade, I have been collecting data about my effectiveness. My outcomes suggest that I’m achieve more than 65% more likely to achieve reliable improvement (71% vs. 43%) with my patients, and about 72% less dropout rates than the average clinician (13% vs. 47%). In addition, contrary to the conventional wisdom that meaningful change takes longer rather than shorter time, my data suggest that my average client experiences reliable improvement between the 3rd or 4th visit, and thus more like to experience gains in subsequent sessions.
Now, our team at Henry Street Centre systematically measuring our outcomes and using that data for improvement. As the research points, this increases the chance of a successful outcome with our clients.
Quick Tips
Before your enter therapy, ask your psychologist/counsellor, “Do you systematically monitor patient outcomes in your practice?”:
While it is crucial to apply an evidence-based approach, it is equally important that clinicians adopt a practice-based evidence approach in the field of psychotherapy. You want to see a therapist who have amassed their own evidence, and not simply claim effectiveness based on borrowed evidence from clinical trials, remote from actual clinical practice.
It’s the therapist, not the type of therapy:
Contrary to popular belief, the variability in outcomes due to the differences between therapist is 5-9 times more than the differences in treatment modality. In other words, it’s not the type of treatment model the therapist endorses or adheres strictly to a type of program (cognitive behavioural, psychodynamic, etc.) that accounts for the good outcomes. Rather, repeated studies and meta-analysis has shown that it is due to who the therapist is (Wampold & Imel, 2015), and what he/she does to develop their level of expert performance (Chow et al., 2015).
In other words, don’t let anyone convince you that they are effective simply because they claim to be doing “evidence-based” practice. The proof of the pudding is in the eating. If not, ask, “Show me your evidence.”
Surprising Fact #3: Client’s age, gender, diagnosis, and previous history of treatment do not predict outcomes.
This may not come as a surprise. Yet, we must not confuse clarity with triviality. Therapist’s experience, professional discipline, and types of therapy models do not predict outcomes. The only factor that is within the locus of control by the therapist to improve outcomes consistently is the engagement of deliberate practice (Ericsson et al., 1993; Chow et al., 2016).
Request for a brief patient-focused outcome feedback from your treating psychologist:
Most GPs I know care about their patients and appreciate some brief updates. They typically like a periodic brief progress report on how the patient is progressing. I urge GPs to request for some form of outcomes based not just on symptoms, but on a patient-rated global wellbeing measure (e.g., Outcome Rating Scale, Clinical Outcome Routine Evaluation, Outcome Questionnaire-45). That way, we can provide a more coherent and integrative care for our patients, especially for those who are receiving a combination of pharmaceutical and psychological interventions.
Boy overjoyed with a new pair of shoes
Like the images of the two boy in this post, I hope you get the help you deserve, and to experience a renewed sense of joy in your life.
Best,
Daryl Chow, PhD
You might also be keen to read from my other blog, Frontiers of Psychotherapist Development:
Why Our Self-Assessment Might be a Delusion of Reality
Clinical Practice vs. Deliberate Practice: Why Your Years of Experience Doesn’t Get You Better
Recent Articles:
Is Your Gut The Second Brain?
The Age of Anxiety
The Physical Effects of Depression
Thank you for subscribing to The Mind of Health. Feel Free (it's free) to browse around and add your comments.